Let the recovery begin
insurance
We provide a no-cost/no-commitment verification of your insurance.
Verifying your insurance is fast and worry-free.
In Network Providers

Other insurance plans we may accept

Let your journey of recovery start now! Learn more about the insurance providers that Free by the Sea will work with in order to provide you or a loved one with premier addiction treatment services. Reaching out is the first step in getting the help you need.
Free by the Sea Is In-Network With the Following Insurance Providers
- Blue Cross Blue Shield
- First Health
- First Choice Health
- Health Smart
- Kaiser Permanente
- HMA
- Pacific Source
- Regence Group Administrators
- Providence Health Plans
- Anthem Blue Cross
- Blue Shield of California
- Beacon Health Options
- MultiPlan
- Blue Cross Blue Shield of Illinois
- Asuris Northwest Health
Other Insurance Plans We May Accept Include:
- GEHA
- UMR
- United Healthcare
- Moda Health
- EBMS
- Aetna
- Cigna
- HealthComp
- United Behavioral Health
- Premera Blue Cross
How Do I Determine My Insurance Coverage for Addiction Treatment?
Determining insurance coverage for addiction treatment can be complex, but here are some general steps to follow:
- Contact your insurance provider: Call your insurance company and ask about your benefits for addiction treatment. Be sure to have your policy number and any other relevant information on hand.
- Ask about in-network providers: In-network providers are typically covered at a higher rate than out-of-network providers, so ask for a list of in-network facilities or professionals.
- Check coverage levels: Your insurance may cover specific types of addiction treatment, such as detoxification or outpatient therapy, but not others like residential treatment programs. Make sure you understand what is covered and what is not.
- Understand deductibles and co-pays: Depending on your plan, you may be responsible for paying a deductible or co-pay before insurance starts covering the costs of addiction treatment.
- Get pre-authorization if needed: Some insurance plans require pre-authorization before they will cover certain types of treatment, so make sure you understand any pre-authorization requirements.
Navigating insurance coverage for addiction treatment can be overwhelming, but don’t hesitate to reach out to your healthcare provider or an addiction specialist for help understanding your options.
What Treatment Services Are Typically Covered by Insurance for Behavioral Health?
The specific treatment services covered by insurance for behavioral health can vary depending on the individual’s insurance plan and provider. However, here are some common types of behavioral health services that may be covered:
- Outpatient therapy: This includes individual or group counseling sessions with a mental health professional.
- Inpatient or residential treatment: If an individual requires intensive treatment, such as for a severe mental illness or substance use disorder, inpatient hospitalization may be covered.
- Prescription medications: Insurance plans may cover prescription medications used to treat mental health conditions, such as antidepressants or antipsychotics.
- Intensive outpatient programs (IOPs): IOPs provide structured treatment for individuals who require more support than outpatient therapy but do not need inpatient care.
- Partial hospitalization programs (PHPs): PHPs are similar to IOPs but provide more intensive treatment and medical monitoring.
- Mental health or dual diagnosis conditions: If an individual requires specialized care for a mental illness or a substance use disorder that co-occurs with mental illness.
It is important to note that not all insurance plans cover all of these services, and coverage levels can vary widely. It’s best to contact your insurance provider directly to understand what specific behavioral health services are covered under your plan.
What Is the Patient Protection and Affordable Care Act?
The Patient Protection and Affordable Care Act (ACA) includes provisions that impact addiction treatment by requiring insurance companies to cover substance use disorder treatment as an essential health benefit. This means that insurance plans must cover the cost of addiction treatment services, including detoxification, rehabilitation, and ongoing support.
The ACA also requires insurance plans to provide coverage for mental health services on par with physical health services. This is known as parity in mental health and substance use disorder benefits, which means that insurers cannot impose more restrictive limitations on behavioral health care than they do on medical or surgical care.
Overall, the ACA has expanded access to addiction treatment services for many individuals who previously could not afford or access this type of care. However, it’s important to note that the specifics of coverage vary depending on the individual’s insurance plan and provider. It’s best to contact your insurance provider directly to understand what specific addiction treatment services are covered under your plan.
What Does It Mean if Free by the Sea Is “In-Network” With My Insurance Provider?
If Free by the Sea is “in-network” with your insurance company, it means that they have a contract or agreement with your insurance provider to provide addiction treatment services at a negotiated rate. This can be beneficial for you as a patient because it may mean lower out-of-pocket costs for treatment.
Additionally, if Free by the Sea is in-network with your insurance company, they will typically handle the billing and paperwork associated with your treatment directly with the insurer. This can simplify the payment process and reduce stress during an already difficult time.
It’s important to note that not all insurance plans cover addiction treatment services, and even if they do, coverage levels can vary widely. It’s best to contact both your insurance provider and Free by the Sea directly to understand what specific addiction treatment services are covered under your plan and what costs you may be responsible for paying out-of-pocket.
Reach Out to Free by the Sea Today!
We provide a no-cost/no-commitment verification of your insurance. We understand for some people, having insurance can be the only reason an individual is able to receive treatment. Therefore, we work diligently to expedite the insurance verification process. We want you to be able to begin the admissions process as soon as possible. Our programs can help return you back to a happy and healthy life.
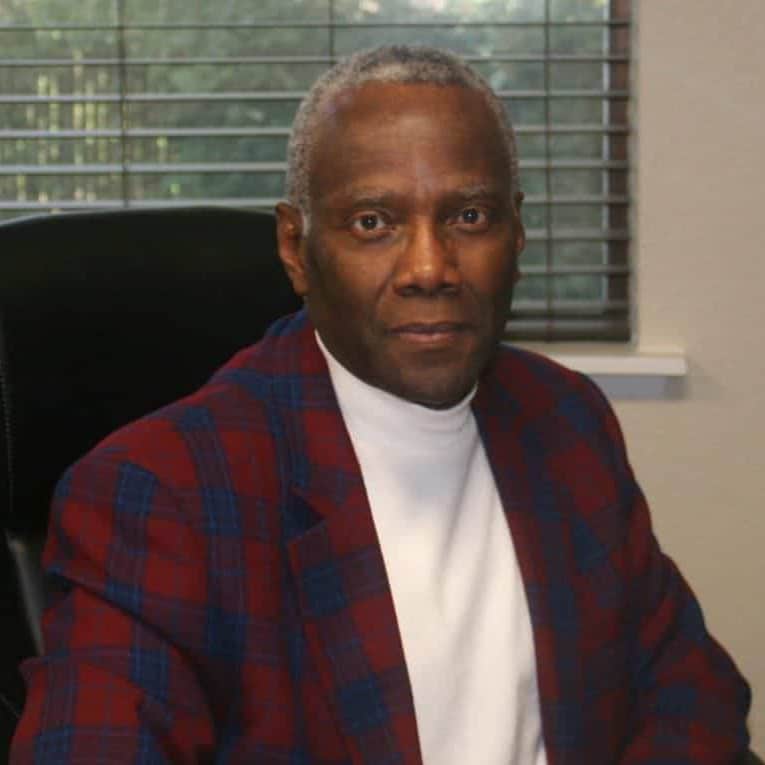
Dr. Richard Crabbe joined our team in 2019 as our psychiatrist and medical director. He attended the University of Ghana Medical School where he became a Medical Doctor in 1977. From 1978 through 1984, he was a medical officer in the Ghana Navy and provided a variety of services from general medicine to surgeries. He received his Certificate in General Psychology from the American Board of Psychology and Neurology in 2002.